Understanding Hepatic Hernias: Causes, Symptoms, and Treatment Options.
A hepatic hernia is a rare condition where liver tissue protrudes through an abnormal opening in the abdominal wall or diaphragm. Here’s a detailed look at the condition:
Types of Hepatic Hernias
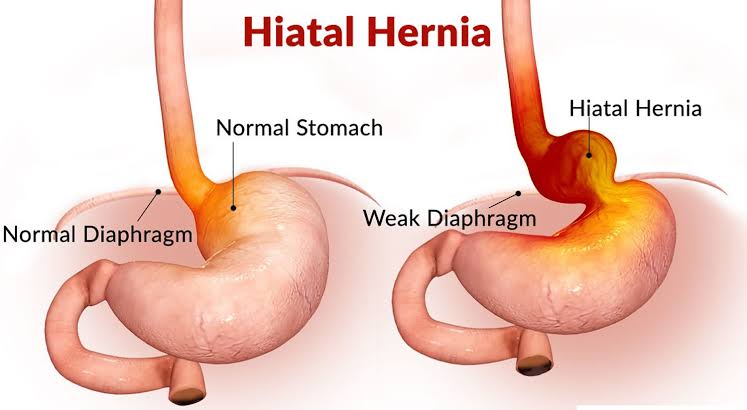
- Diaphragmatic Hernia: This occurs when liver tissue pushes through a defect or weakness in the diaphragm, the muscle that separates the chest from the abdomen.
- Abdominal Wall Hernia: This happens when liver tissue bulges through a weakened area of the abdominal wall.
Causes and Risk Factors
- Congenital Defects: Some people are born with weaknesses in their diaphragm or abdominal wall that predispose them to hernias.
- Trauma or Injury: Trauma to the abdominal area can lead to the development of a hernia.
- Increased Abdominal Pressure: Conditions that increase intra-abdominal pressure, such as chronic coughing, heavy lifting, or obesity, can contribute to hernia formation.
- Surgical Complications: Past abdominal surgery can sometimes lead to hernia formation.
Symptoms
Symptoms can vary depending on the hernia’s location and severity but may include:
- Abdominal pain or discomfort
- Swelling or bulging in the abdomen or chest
- Nausea or vomiting
- Difficulty breathing (if the hernia affects the diaphragm)
Diagnosis
Diagnosis typically involves a combination of:
- Physical Examination: A doctor may detect a bulge or abnormality during a physical exam.
- Imaging Studies: Techniques like ultrasound, CT scans, or MRI can help visualize the hernia and determine its extent.
Treatment
Treatment options depend on the hernia’s size, symptoms, and the patient’s overall health:
- Surgical Repair: The primary treatment is usually surgical correction, which involves repairing the defect in the abdominal wall or diaphragm. This can be done through traditional open surgery or minimally invasive laparoscopic techniques.
- Supportive Measures: In some cases, supportive measures like wearing a hernia belt or making lifestyle changes to reduce abdominal pressure may be recommended, especially if surgery isn’t immediately necessary.
Prognosis
With appropriate treatment, the prognosis for hepatic hernias is generally good. However, complications can arise if the hernia is not treated, such as strangulation (where the blood supply to the herniated tissue is cut off) or incarceration (where the hernia becomes trapped and cannot be pushed back into place)
Hepatic hernia causes:
1. Congenital Defects
- Diaphragmatic Hernia: A congenital defect where the diaphragm has an abnormal opening present from birth, allowing liver tissue to push through.
- Abdominal Wall Defects: Rare congenital conditions where the abdominal wall has weaknesses or defects that can lead to a hernia.
2. Trauma or Injury
- Abdominal Trauma: Physical injury or trauma to the abdomen, such as from accidents or severe impacts, can cause or exacerbate a hernia.
- Surgical Trauma: Previous abdominal surgery might weaken the abdominal wall or diaphragm, increasing the risk of a hernia.
3. Increased Intra-Abdominal Pressure
- Heavy Lifting: Repeated heavy lifting or strenuous physical activities can increase pressure within the abdomen, potentially leading to a hernia.
- Chronic Coughing: Persistent coughing from conditions like chronic bronchitis or asthma can elevate abdominal pressure and contribute to hernia formation.
- Obesity: Excess weight puts additional pressure on the abdominal wall and diaphragm, which can lead to hernias over time.
4. Weaknesses in Abdominal Structures
- Aging: As people age, the abdominal wall and diaphragm can become weaker and more prone to hernia formation.
- Genetic Predisposition: Some individuals may have a genetic predisposition to weaker connective tissues, making them more susceptible to hernias.
5. Abdominal Conditions
- Pregnancy: The physical changes and increased abdominal pressure during pregnancy can contribute to hernia development.
- Ascites: Fluid accumulation in the abdomen due to liver disease or other conditions can increase intra-abdominal pressure and lead to hernias.
6. Previous Surgical Procedures
- Post-Surgical Weakness: Incisions from past abdominal surgeries can weaken the abdominal wall, making it easier for a hernia to develop.
- Inadequate Healing: If a previous surgical site does not heal properly or if there is a surgical complication, it can contribute to hernia formation.
7. High-Risk Activities
- Strenuous Exercise: Certain types of exercise, especially those that involve heavy lifting or high abdominal pressure, might contribute to the development of hernias if not done correctly or with proper precautions.
8. Other Medical Conditions
- Chronic Constipation: Straining during bowel movements can increase abdominal pressure and lead to hernia formation.
- Cystic Fibrosis: In some rare cases, conditions like cystic fibrosis, which affect the lungs and digestive system, can also contribute to hernia development due to chronic coughing and increased abdominal pressure.
Treating a hepatic hernia:
1. Surgical Treatment
Surgical intervention is often necessary to repair a hepatic hernia. The specific approach depends on the hernia’s type, size, and severity.
a. Open Surgery
- Procedure: An incision is made in the abdominal wall or diaphragm to access and repair the hernia. The protruding liver tissue is repositioned, and the defect is repaired with sutures or mesh.
- Recovery: Typically involves a longer recovery period compared to minimally invasive techniques. The patient might need to stay in the hospital for several days.
b. Laparoscopic Surgery
- Procedure: Small incisions are made in the abdomen, and a laparoscope (a thin tube with a camera) is used to guide the repair. Special instruments are used to fix the hernia and reinforce the defect.
- Recovery: Generally faster and less painful than open surgery, with a shorter hospital stay and quicker return to normal activities.
2. Non-Surgical Management
In cases where surgery is not immediately feasible or advisable, non-surgical management can help alleviate symptoms and prevent the hernia from worsening.
a. Hernia Belts or Supports
- Purpose: Hernia belts or abdominal supports can provide external pressure to keep the hernia in place and reduce discomfort. However, they are not a cure and should be used as a temporary measure.
b. Lifestyle Modifications
- Weight Management: Reducing body weight can help decrease abdominal pressure and prevent the hernia from worsening.
- Avoiding Heavy Lifting: Modifying activities to avoid heavy lifting or straining can help prevent additional pressure on the hernia.
c. Dietary Changes
- High-Fiber Diet: Eating a diet high in fiber can help manage constipation and reduce strain during bowel movements, which can contribute to hernia development.
3. Addressing Underlying Conditions
Treating any conditions that might have contributed to the hernia is important for preventing recurrence and managing overall health.
- Chronic Cough: If a chronic cough is a contributing factor, addressing the underlying cause (e.g., treating asthma or chronic bronchitis) can reduce abdominal pressure.
- Ascites Management: If fluid buildup in the abdomen is a factor, managing the underlying liver disease and controlling ascites can help.
4. Post-Surgical Care
Post-surgical care is crucial for a successful recovery and to prevent complications:
- Follow-Up Appointments: Regular follow-ups with your surgeon are important to monitor healing and ensure that the hernia has been effectively repaired.
- Pain Management: Pain relief and management, as prescribed by the doctor, to ensure comfort during recovery.
- Gradual Return to Activity: Following the surgeon’s recommendations for gradually resuming physical activity and avoiding strenuous exercises until fully healed.
5. Choosing the Right Healthcare Facility
- Specialized Centers: Advanced hospitals and surgical centers with expertise in hernia repairs can offer the best treatment options. In India, major cities like Delhi, Mumbai, Bangalore, and Chennai have reputed hospitals with specialized departments for hernia management.
Hepatic Hernia Treatment In India:
. Diagnosis and Evaluation
Before treatment, a thorough diagnosis is necessary. In India, diagnostic procedures might involve:
- Physical Examination: Conducted by a general surgeon or gastroenterologist.
- Imaging Studies: Ultrasound, CT scans, or MRI, available at various diagnostic centers across the country.
2. Treatment Options
Surgical Intervention:
- Open Surgery: This traditional approach involves making a larger incision to repair the hernia. It’s performed in many hospitals and is well-established in India.
- Laparoscopic Surgery: Minimally invasive surgery using small incisions and a camera. It’s often preferred for its quicker recovery times and less post-operative discomfort. Many advanced hospitals and clinics in urban areas offer laparoscopic options.
Healthcare Facilities:
- Major Hospitals: Renowned hospitals like Apollo Hospitals, Fortis Healthcare, and Max Healthcare, as well as many other private and public hospitals, are equipped to handle complex surgical procedures, including hernia repairs.
- Specialty Clinics: Clinics specializing in gastrointestinal or hernia surgery can provide expert care, particularly in metropolitan areas.
Post-Surgical Care:
- Follow-Up: Regular follow-ups are essential to monitor recovery and ensure the hernia has been adequately repaired. These are typically arranged by the treating surgeon or hospital.
- Rehabilitation: Guidance on lifestyle modifications, physical therapy if needed, and dietary recommendations to support healing and prevent recurrence.
3. Non-Surgical Management
For patients who may not be immediately suitable for surgery, such as those with significant comorbidities:
- Supportive Measures: Use of hernia belts or braces to manage symptoms.
- Lifestyle Adjustments: Recommendations to reduce abdominal pressure, including weight management and avoiding heavy lifting.
4. Costs and Accessibility
- Public Healthcare: Government hospitals offer treatment at lower costs, though the availability of specialized care might vary.
- Private Healthcare: Private hospitals generally offer faster service and more advanced facilities but at a higher cost. Many patients opt for private care to access the latest technology and specialized expertise.
5. Finding a Specialist
To find a specialist or suitable treatment facility in India:
- Consultation: Seek referrals from general practitioners or primary care doctors.
- Online Research: Look for top-rated hospitals or clinics in major cities like Delhi, Mumbai, Bangalore, Chennai, or Hyderabad.
- Medical Tourism: Some international patients travel to India for treatment due to its high-quality care and relatively lower costs.
6. Insurance and Financial Considerations
- Health Insurance: Check if your insurance covers surgical procedures and related treatments. Many insurance plans in India cover hernia surgeries.
- Payment Plans: Some hospitals offer payment plans or financial assistance to help manage treatment costs.
