Understanding Diverticulitis
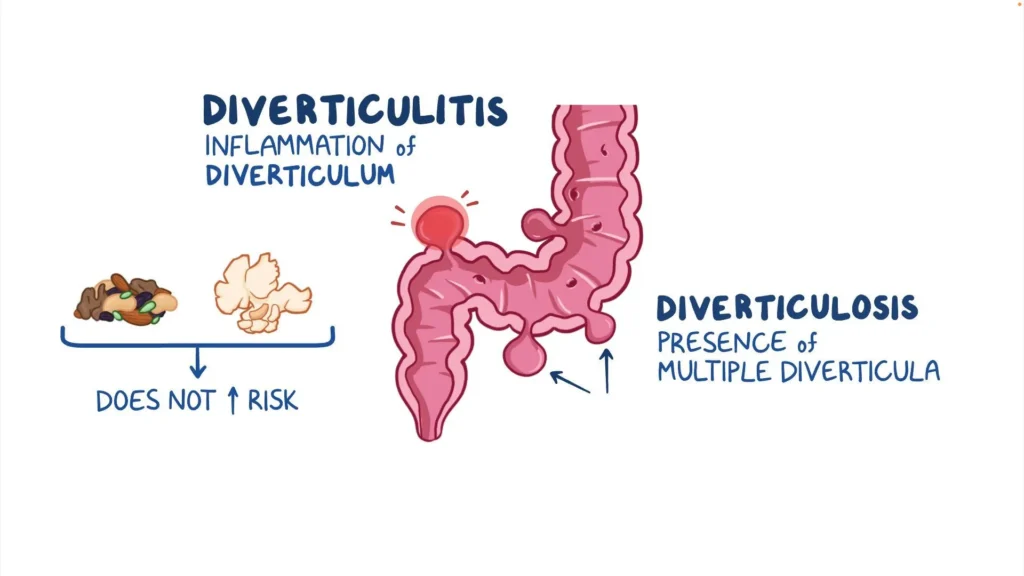
Diverticulitis is a condition that occurs when small pouches (diverticula) that can form in the walls of the colon become inflamed or infected. Here’s a comprehensive overview:
Causes
The causes of diverticulitis primarily relate to the formation of diverticula and subsequent inflammation or infection. Here are the key factors:
1. Diverticula Formation
- Increased Pressure: The colon’s muscular walls can thicken and bulge under pressure, forming pouches (diverticula).
- Low-Fiber Diet: A diet low in fiber can lead to constipation, which increases pressure in the colon as stool becomes harder and more difficult to pass.
2. Inflammation/Infection
- Trapped Fecal Matter: When stool or undigested food gets trapped in a diverticulum, it can lead to inflammation or infection.
- Bacterial Growth: The stagnant stool can allow bacteria to multiply, resulting in diverticulitis.
3. Other Contributing Factors
- Age: The risk increases with age, as the strength and elasticity of the colon decrease.
- Obesity: Excess body weight can contribute to increased pressure on the colon.
- Smoking: Tobacco use is linked to a higher risk of diverticulitis.
- Sedentary Lifestyle: Lack of physical activity can impact bowel function and contribute to constipation.
4. Genetic Factors
- Family History: A family history of diverticular disease can increase individual risk.
Understanding these causes can help in making dietary and lifestyle changes that may reduce the risk of developing diverticulitis.
Risk factors
1. Age
- The risk increases significantly after the age of 40, with most cases occurring in older adults.
2. Diet
- Low Fiber Intake: Diets lacking in fiber can lead to constipation and increased pressure in the colon, contributing to diverticula formation.
3. Obesity
- Being overweight or obese increases the likelihood of developing diverticulitis due to added pressure on the colon.
4. Smoking
- Tobacco use is linked to a higher risk of diverticular disease and complications.
5. Sedentary Lifestyle
- Lack of physical activity can lead to slower bowel movements and increased risk of constipation.
6. Family History
- A family history of diverticular disease can increase individual susceptibility.
7. Certain Medications
- Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, and steroids may raise the risk.
8. Chronic Conditions
- Conditions such as diabetes or connective tissue disorders can also be associated with a higher risk.
Awareness of these risk factors can help in making informed lifestyle choices to potentially reduce the risk of developing diverticulitis.
The symptoms of diverticulitis
1. Abdominal Pain
- Typically located in the lower left quadrant of the abdomen.
- The pain may be sudden and severe or gradual and mild.
2. Fever
- Often present, indicating inflammation or infection.
3. Nausea and Vomiting
- Can occur, especially if the condition is more severe.
4. Change in Bowel Habits
- May include constipation or diarrhea.
- Some individuals may experience alternating patterns.
5. Bloating and Gas
- Discomfort and a feeling of fullness in the abdomen.
6. Loss of Appetite
- Due to discomfort and gastrointestinal distress.
7. Tenderness in the Abdomen
- A physical exam may reveal tenderness, particularly in the lower left side.
8. Rectal Bleeding
- Although less common, some may experience bleeding from the rectum.
If you experience severe abdominal pain, fever, or other significant symptoms, it’s important to seek medical attention promptly, as these can indicate complications.
Diagnosing diverticulitis
1. Medical History
- Symptom Review: Discussion of symptoms, their duration, and severity.
- Past Medical History: Evaluation of any previous episodes of diverticulitis or other gastrointestinal conditions.
2. Physical Examination
- Abdominal Exam: The healthcare provider checks for tenderness, particularly in the lower left abdomen, and may assess for signs of a mass or rigidity.
3. Imaging Tests
- CT Scan:
- This is the most common and effective test for diagnosing diverticulitis. It can reveal inflamed diverticula, abscesses, and complications.
- Ultrasound:
- May be used in some cases, especially in pregnant women, as it avoids radiation exposure.
- X-ray:
- Generally less useful for diverticulitis but may help rule out other conditions like bowel obstruction.
4. Blood Tests
- Complete Blood Count (CBC):
- Can show elevated white blood cell counts, indicating infection or inflammation.
- Other Tests:
- May be done to assess overall health and rule out other conditions.
5. Colonoscopy
- Typically not performed during an acute episode due to the risk of perforation but may be done later to rule out other colon diseases.
Conclusion
If diverticulitis is suspected, timely diagnosis is crucial to initiate appropriate treatment and avoid complications. Always consult a healthcare professional if experiencing symptoms.
Treatment
1. Mild Cases
- Dietary Changes:
- Initially, a clear liquid diet may be recommended to allow the colon to rest. Gradually, low-fiber foods can be reintroduced, followed by high-fiber foods as symptoms improve.
- Antibiotics:
- Oral antibiotics may be prescribed to treat any infection.
- Pain Management:
- Over-the-counter pain relievers (like acetaminophen) may be used. Avoid NSAIDs (like ibuprofen) as they can increase the risk of complications.
2. Moderate to Severe Cases
- Hospitalization:
- If symptoms are severe or complications arise, hospitalization may be necessary.
- Intravenous (IV) Antibiotics:
- Administered to treat infection more effectively.
- IV Fluids:
- To prevent dehydration and maintain nutrition if oral intake is not possible.
3. Surgical Treatment
- Surgery may be necessary for:
- Complications: Such as abscesses, perforation, or fistulas.
- Recurrent Diverticulitis: If someone has multiple episodes, surgical intervention might be considered.
- Types of Surgery:
- Resection: Removal of the affected portion of the colon. This may involve creating a temporary colostomy, which is often reversed later.
- Drainage: In cases of abscess formation, a minimally invasive procedure to drain the abscess may be performed.
4. Long-Term Management
- Dietary Adjustments:
- After recovery, a high-fiber diet is recommended to prevent future episodes. This includes fruits, vegetables, whole grains, and plenty of fluids.
- Regular Exercise:
- Promotes bowel health and reduces the risk of constipation.
- Routine Follow-ups:
- Monitoring by a healthcare provider for any signs of recurrence or complications.
Conclusion
The appropriate treatment for diverticulitis will depend on individual circumstances, and it’s essential to work closely with a healthcare provider for personalized care. If symptoms persist or worsen, seek medical attention promptly.
Preventing diverticulitis
1. High-Fiber Diet
- Increase Fiber Intake: Aim for 25-30 grams of fiber daily from fruits, vegetables, whole grains, legumes, and nuts. Fiber helps to soften stool and prevent constipation, reducing pressure in the colon.
2. Hydration
- Drink Plenty of Fluids: Staying well-hydrated aids digestion and helps fiber work effectively. Aim for at least 8 cups (about 2 liters) of water daily.
3. Regular Exercise
- Stay Active: Engaging in regular physical activity helps maintain healthy bowel function and can reduce the risk of constipation.
4. Weight Management
- Maintain a Healthy Weight: Achieving and maintaining a healthy weight can help lower the risk of developing diverticulitis.
5. Avoid Smoking
- Quit Tobacco: Smoking is linked to a higher risk of diverticular disease, so quitting can significantly benefit your overall health.
6. Limit Processed Foods
- Reduce Intake of Low-Fiber Foods: Avoid or limit processed foods, red meat, and foods high in refined sugars and fats, as these can contribute to a low-fiber diet.
7. Moderation in Certain Foods
- Cautious with Seeds and Nuts: While research is mixed, some individuals may choose to avoid small seeds and nuts if they have had diverticulitis, although they are generally considered safe for most people.
8. Regular Medical Check-ups
- Routine Health Assessments: Regular visits to a healthcare provider can help monitor digestive health and identify potential issues early.
Conclusion
By adopting these preventive measures, individuals can significantly reduce their risk of developing diverticulitis. It’s important to consult a healthcare professional for personalized advice, especially if you have a history of diverticular disease.
Complications
- Abscess: Pockets of infection can form.
- Perforation: A hole in the colon, which can lead to serious infections.
- Fistula: An abnormal connection between the colon and other organs.
- Intestinal Obstruction: Scar tissue from inflammation can lead to blockages.
Prognosis
With proper treatment and lifestyle changes, many people can manage diverticulitis effectively. However, recurrent episodes can occur, and serious complications may require surgery.
If you suspect you have diverticulitis or are experiencing symptoms, it’s important to consult a healthcare professional for an accurate diagnosis and appropriate management
