Navigating the Costs and Care: Managing Nipah Virus Infection in India.
Nipah virus is a highly dangerous pathogen with the potential to cause severe disease in both animals and humans. Here’s an overview of the virus:
Overview
- Family: Paramyxoviridae
- Genus: Henipavirus
- Species: Nipah virus (NiV)
Transmission
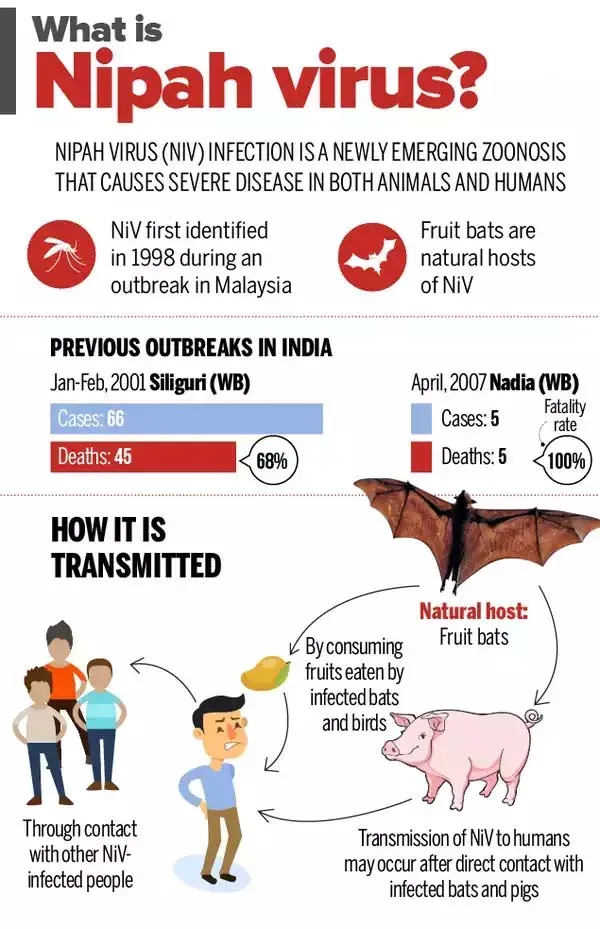
Nipah virus is zoonotic, meaning it can be transmitted from animals to humans. The primary hosts are fruit bats (especially Pteropus species). Transmission can occur through:
- Direct contact with infected bats or their saliva, urine, or feces.
- Consumption of contaminated food, such as fruit contaminated by bat saliva or urine.
- Human-to-human transmission, which is less common but can occur through close contact with infected individuals, particularly in healthcare settings.
Symptoms
Infected individuals may experience a range of symptoms, which can progress rapidly. Early symptoms include:
- Fever
- Headache
- Dizziness
- Muscle pain
As the disease progresses, it can lead to more severe symptoms such as:
- Encephalitis (inflammation of the brain)
- Coma
- Respiratory distress
Incubation Period
The incubation period for Nipah virus is typically 5 to 14 days but can vary. Symptoms usually begin within 5 to 14 days after exposure.
Diagnosis
Diagnosis is challenging and usually involves:
- Clinical evaluation of symptoms and history of exposure.
- Laboratory tests, such as PCR (polymerase chain reaction) to detect viral RNA, and serological tests to identify antibodies.
Treatment
There is no specific antiviral treatment for Nipah virus infection. Supportive care is the primary approach, including:
- Management of symptoms
- Hospitalization for severe cases
- Isolation to prevent spread
Prevention
Preventive measures include:
- Avoiding contact with infected animals or their secretions.
- Ensuring food hygiene, particularly in areas where Nipah virus is known to be present.
- Using protective gear when caring for infected individuals.
Outbreaks
Diagnosis:
Clinical Diagnosis
- Medical History and Symptoms:
- Exposure History: Recent travel to areas with known Nipah virus outbreaks or contact with fruit bats or pigs.
- Symptoms: Initial symptoms may include fever, headache, myalgia (muscle pain), and dizziness. Severe cases can progress to encephalitis, seizures, and coma.
- Clinical Evaluation:
- Physical Examination: Assessment of neurological symptoms, respiratory status, and overall condition.
Laboratory Diagnosis
- Polymerase Chain Reaction (PCR):
- Purpose: Detects viral RNA in blood, cerebrospinal fluid (CSF), or tissue samples.
- Timing: Best performed during the acute phase of the illness, typically within the first week of symptoms.
- Serological Tests:
- Purpose: Detects antibodies against the Nipah virus. This includes:
- Enzyme-Linked Immunosorbent Assay (ELISA): To identify specific antibodies (IgM and IgG) against Nipah virus.
- Indirect Immunofluorescence Assay (IFA): Used for detecting viral proteins and antibodies.
- Timing: Antibody tests are useful after the first week of illness, as antibodies may not be detectable in the early stages.
- Purpose: Detects antibodies against the Nipah virus. This includes:
- Virus Isolation:
- Purpose: To culture the virus from clinical samples, although this method is less commonly used due to its complexity and biohazard risks.
- Immunohistochemistry:
- Purpose: Detects viral antigens in tissue samples, particularly in autopsy specimens, but is less commonly used for live patients.
Challenges in Diagnosis
- Similarities to Other Diseases: Nipah virus infection can present with symptoms similar to other viral encephalitides or respiratory illnesses, which can complicate diagnosis.
- Limited Availability of Testing: In some regions, specialized tests like PCR and serology might not be readily available.
Confirmation and Management
- Confirmation: Diagnosis is confirmed by detecting viral RNA or antibodies specific to Nipah virus.
- Management: Once diagnosed, supportive care is essential, and isolation precautions should be taken to prevent transmission.
CAUSE:
1. Origin and Host
- Natural Reservoir: The primary host for Nipah virus is fruit bats, especially species from the genus Pteropus, commonly known as flying foxes. These bats carry the virus without showing symptoms.
- Intermediate Hosts: Infected bats can transmit the virus to other animals, notably pigs, which have been implicated in outbreaks. Pigs can then act as intermediate hosts, amplifying the virus before it spreads to humans.
**2. Transmission Pathways
- Animal-to-Human Transmission:
- Direct Contact: Humans can become infected through direct contact with bodily fluids (like saliva, urine, or feces) from infected bats or pigs.
- Contaminated Food: Consumption of fruits or fruit products contaminated with bat saliva or urine can also lead to infection.
- Human-to-Human Transmission:
- Close Contact: The virus can spread from person to person through close physical contact with bodily fluids of an infected individual. This is particularly notable in healthcare settings or among family members caring for the infected.
- Respiratory Droplets: There is some evidence that respiratory droplets from an infected person might contribute to transmission, but this is less well-documented.
**3. Environmental Factors
- Ecological and Agricultural Practices: In regions where Nipah virus is endemic, deforestation and intensive agriculture can increase the likelihood of bat-human contact. For example, pigs and bats may come into contact more frequently in such settings, increasing the risk of spillover events.
**4. Virus Characteristics
- Viral Structure: Nipah virus is an enveloped, single-stranded RNA virus belonging to the genus Henipavirus. Its ability to cause severe disease in multiple species is partly due to its capacity to affect the endothelial cells lining blood vessels, leading to systemic disease.
**5. Outbreaks and Epidemiology
- Geographic Distribution: Nipah virus outbreaks have been reported primarily in South and Southeast Asia. The first major outbreak occurred in Malaysia in 1998-1999, with subsequent outbreaks in Bangladesh and India.
Symptoms:
Initial Symptoms
- Fever: Often the first symptom, characterized by high temperature.
- Headache: Severe headaches are common.
- Muscle Pain: Myalgia or muscle pain is frequently reported.
- Dizziness: Individuals may experience dizziness or lightheadedness.
- Fatigue: General malaise and tiredness are typical.
Progressive Symptoms
If the disease progresses, the symptoms can become more severe and include:
- Encephalitis: Inflammation of the brain, which may present as confusion, altered mental status, and seizures.
- Seizures: Neurological symptoms such as seizures can occur.
- Coma: In severe cases, the patient may fall into a coma.
- Respiratory Distress: Some individuals may develop respiratory symptoms, including cough and difficulty breathing.
Severe and Complicated Cases
In advanced stages, complications may arise:
- Neurological Complications: Severe cases may involve permanent neurological damage or long-term cognitive impairment.
- Respiratory Failure: In severe respiratory cases, the patient may need mechanical ventilation.
- Death: The mortality rate can be high, with fatalities often resulting from severe encephalitis or complications like secondary infections.
Symptoms in Animals
In animals such as pigs, the symptoms can include:
- Acute Respiratory Disease: Including coughing, nasal discharge, and difficulty breathing.
- Neurological Signs: Some animals may exhibit signs like incoordination or tremors.
Variability and Incubation Period
- Incubation Period: Symptoms typically appear 5 to 14 days after exposure, but this can vary.
- Variability: The severity and specific symptoms can vary based on the individual’s health, age, and immune status.
Prevention:
**1. Avoiding Contact with Potential Reservoirs
- Fruit Bats:
- Avoid Areas with High Bat Activity: In regions where Nipah virus is known to be present, avoid contact with bats or areas where bats roost.
- Protective Measures: Use protective clothing and equipment if working in environments where contact with bats might occur.
- Pigs:
- Avoid Contact: Avoid close contact with pigs, especially in areas experiencing outbreaks.
- Biosecurity Measures: Implement biosecurity measures on farms to prevent the introduction and spread of the virus among animals.
**2. Food Safety
- Avoid Contaminated Food:
- Fruit: Do not consume fruits that may have been contaminated with bat saliva or urine.
- Food Preparation: Wash fruits and vegetables thoroughly before consumption.
- Proper Handling and Cooking:
- Meat: Ensure that meat, particularly from pigs, is thoroughly cooked. Avoid eating raw or undercooked meat.
**3. Hygiene and Infection Control
- Hand Hygiene:
- Frequent Hand Washing: Wash hands regularly with soap and water, especially after contact with animals or their secretions.
- Hand Sanitizers: Use alcohol-based hand sanitizers if soap and water are not available.
- Protective Equipment:
- PPE: In areas with Nipah virus outbreaks, use personal protective equipment (PPE) such as gloves, masks, and gowns when caring for infected individuals or handling potentially contaminated materials.
**4. Infection Control in Healthcare Settings
- Isolation:
- Infected Patients: Isolate patients with suspected or confirmed Nipah virus infection to prevent transmission.
- Strict Infection Control: Follow stringent infection control practices, including the use of PPE, to protect healthcare workers and other patients.
- Sterilization:
- Equipment: Ensure that medical and laboratory equipment is properly sterilized.
**5. Community and Public Health Measures
- Public Awareness:
- Education: Educate communities about the risks of Nipah virus and the importance of avoiding contact with bats and pigs.
- Alert Systems: Implement and follow public health alerts and advisories in areas experiencing outbreaks.
- Surveillance and Reporting:
- Monitoring: Monitor and report cases of Nipah virus to public health authorities to enable rapid response and containment efforts.
**6. Research and Vaccination
- Ongoing Research:
- Vaccines: Support research into vaccines and treatments for Nipah virus to enhance long-term prevention strategies.
- Outbreak Preparedness: Participate in and support efforts to develop and implement outbreak response plans.
TREATMENT IN INDIA:
*1. Supportive Care
- Hospitalization: Patients with Nipah virus infection typically require hospitalization, particularly those with severe symptoms such as encephalitis or respiratory distress.
- Symptomatic Treatment:
- Fever and Pain Management: Antipyretics (such as paracetamol) and analgesics are used to manage fever and pain.
- Hydration: Intravenous fluids may be administered to maintain hydration and electrolyte balance.
- Monitoring: Continuous monitoring of vital signs and neurological status is essential for severe cases.
**2. Management of Complications
- Encephalitis:
- Neuroprotection: Patients with encephalitis may require neuroprotective measures and medications to manage seizures and reduce brain inflammation.
- Supportive Neurological Care: Specialist care, including neurologists, may be involved in managing severe neurological symptoms.
- Respiratory Support:
- Ventilation: For patients with severe respiratory distress or failure, mechanical ventilation may be necessary.
**3. Infection Control
- Isolation:
- Prevent Transmission: Infected patients are isolated to prevent the spread of the virus to healthcare workers and other patients.
- PPE Use: Healthcare workers use personal protective equipment (PPE) to reduce the risk of transmission.
- Sterilization: Proper sterilization of medical equipment and thorough cleaning of the patient’s environment are critical.
**4. Preventive Measures
- Contact Tracing and Quarantine: In the event of an outbreak, contact tracing and quarantine measures may be implemented to prevent further spread.
**5. Research and Experimental Treatments
- Ongoing Research: Research into antiviral drugs and vaccines is ongoing, and new treatments may become available as they are developed and tested.
- Clinical Trials: Participation in clinical trials for experimental treatments and vaccines may be an option for some patients, though this is subject to availability and approval.
**6. Public Health and Advisory
- Guidelines: The Indian government and public health authorities provide guidelines for managing Nipah virus cases, including recommendations for healthcare facilities and emergency response.
- Awareness: Efforts are made to raise awareness among healthcare providers and the public about the symptoms, prevention, and management of Nipah virus infection.
Treatment Centers
- Specialized Centers: In India, specialized treatment may be available at major hospitals and research institutions equipped to handle high-risk infections, including those with expertise in infectious diseases and critical care.
TREATMENT COST:
. Hospitalization
- General Ward: Costs for hospitalization in a general ward can vary widely depending on the facility. In government hospitals, costs may be lower compared to private hospitals.
- ICU Care: For severe cases requiring intensive care unit (ICU) admission, costs are significantly higher. ICU care includes advanced monitoring, specialized medical equipment, and potentially life support systems.
**2. Supportive Care
- Medication: The cost of medications for symptom management, such as antipyretics, analgesics, and any additional drugs required for managing complications, can add to the overall expense.
- Intravenous Fluids: Administration of IV fluids and electrolytes is a common part of supportive care and can contribute to costs.
**3. Diagnostic Testing
- Laboratory Tests: Diagnostic tests, including PCR assays, serology, and imaging studies (such as CT or MRI scans), can be expensive, especially if advanced diagnostic facilities are used.
- Specialist Consultations: Fees for consultations with specialists, such as neurologists or intensivists, may be incurred.
**4. Infection Control Measures
- Isolation and PPE: Costs related to infection control, including isolation protocols and the use of personal protective equipment (PPE) by healthcare workers, can contribute to the total expense.
**5. Additional Costs
- Travel and Accommodation: For patients needing specialized care or traveling from remote areas, costs can include transportation and accommodation.
- Support Services: Additional costs may include physiotherapy, psychological support, and long-term rehabilitation if needed.
Cost Estimates
- Government Hospitals: Treatment in government hospitals may be more affordable, with costs potentially ranging from a few thousand to several tens of thousands of Indian Rupees (INR) depending on the severity of the case and the length of hospital stay.
- Private Hospitals: Private hospitals generally have higher costs, which can range from tens of thousands to several lakhs of INR, particularly for ICU and specialized care.
Insurance Coverage
- Health Insurance: The extent of coverage for Nipah virus treatment under health insurance policies can vary. It’s advisable to check with insurance providers to understand coverage limits and out-of-pocket expenses.
Financial Assistance
- Government and NGO Support: In some cases, government or non-governmental organizations (NGOs) may provide financial assistance or subsidies for patients from low-income backgrounds.
