Navigating Rosacea: A Comprehensive Guide
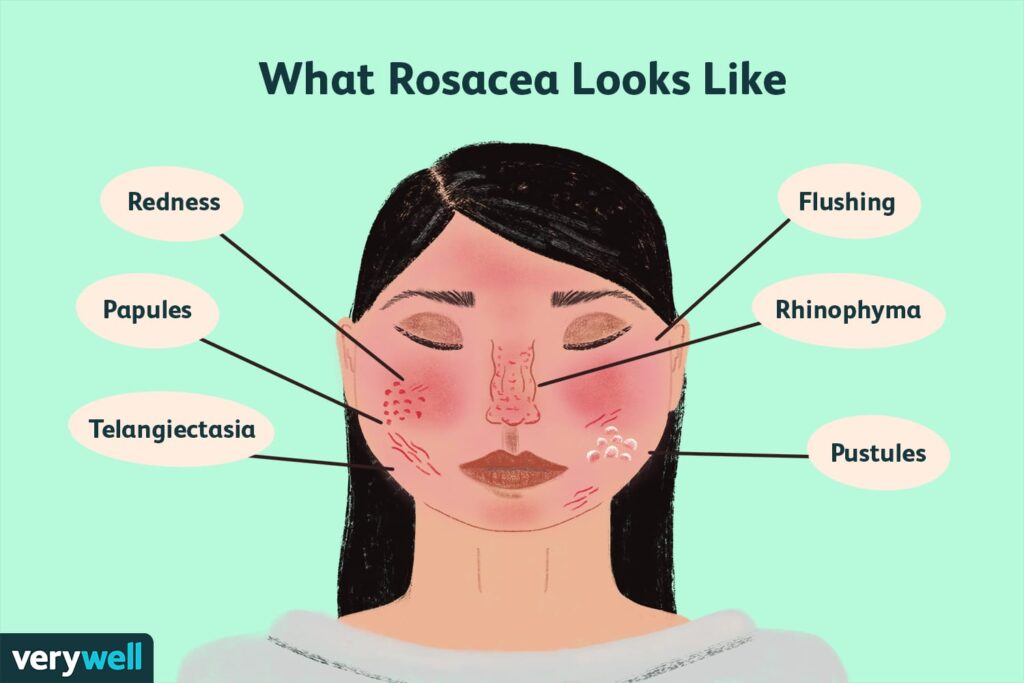
Rosacea is a chronic skin condition that primarily affects the face, causing redness, visible blood vessels, and sometimes acne-like bumps. Here’s an in-depth look at rosacea:
Symptoms
1. Erythematotelangiectatic Rosacea
- Facial Redness: Persistent redness in the central part of the face, often appearing as a flush or sunburn.
- Visible Blood Vessels: Small, dilated blood vessels (telangiectasia) that become more noticeable, usually on the cheeks, nose, and chin.
- Skin Sensitivity: The affected skin may feel sensitive or sting, especially in response to temperature changes, skincare products, or sun exposure.
2. Papulopustular Rosacea
- Acne-like Breakouts: Red, swollen bumps that can resemble acne. These may be accompanied by pus-filled pustules.
- Persistent Redness: Similar to erythematotelangiectatic rosacea, with a red base that is visible between and around the bumps.
- Swelling: Some individuals may experience facial swelling, especially around the cheeks and eyes.
3. Phymatous Rosacea
- Thickened Skin: Skin thickening, particularly noticeable on the nose (rhinophyma), which can become enlarged and bulbous.
- Texture Changes: The skin may become rough and bumpy, with an irregular surface.
- Nasal Congestion: In severe cases, the thickening can lead to breathing difficulties through the nose.
4. Ocular Rosacea
- Eye Irritation: Burning, stinging, or itching sensations in the eyes.
- Red or Bloodshot Eyes: The eyes may appear red or bloodshot.
- Dryness: The eyes may feel dry or gritty, sometimes leading to frequent blinking.
- Eyelid Issues: Inflammation of the eyelids (blepharitis) or conjunctivitis (pink eye) can occur.
- Vision Disturbances: In severe cases, rosacea can lead to vision problems if left untreated.
General Symptoms
- Flushing: Episodes of sudden, intense redness or warmth in the face.
- Hot Sensation: A feeling of heat or burning in the facial skin.
- Dryness or Flakiness: Some individuals may experience dryness or flakiness of the affected areas.
Symptom Patterns
- Triggers: Symptoms can be exacerbated by certain triggers such as spicy foods, alcohol, hot beverages, extreme temperatures, or stress.
- Chronic Nature: Symptoms tend to be persistent and may fluctuate in severity, often worsening with time if left untreated.
It’s important to recognize these symptoms early and consult a dermatologist for an accurate diagnosis and appropriate management plan.
Causes
The exact cause of rosacea is not fully understood, but several factors are believed to contribute to its development. Here’s a detailed look at the potential causes and contributing factors:
1. Genetic Factors
- Family History: There is evidence suggesting that rosacea may run in families. Individuals with a family history of rosacea or similar skin conditions may be more likely to develop it.
2. Immune System Abnormalities
- Inflammatory Response: An abnormal immune response may play a role in rosacea. The condition is thought to involve inflammation and an overactive immune system that reacts to triggers inappropriately.
- Demodex Mites: Increased numbers of Demodex mites, which are normally found on the skin, may be associated with rosacea. These mites may trigger inflammatory responses in some people.
3. Blood Vessel Abnormalities
- Vascular Changes: Rosacea is characterized by visible blood vessels and facial flushing. Abnormalities in blood vessels, including their dilation and increased blood flow, may contribute to the symptoms.
- Temperature Sensitivity: The condition can be triggered by temperature changes, suggesting that blood vessel regulation plays a role in its development.
4. Microbial Factors
- Skin Bacteria: Some research suggests that certain skin bacteria might be involved in triggering rosacea. However, the exact relationship is not fully established.
- Helicobacter pylori: There has been speculation that the bacterium Helicobacter pylori, which is associated with gastrointestinal conditions, might be linked to rosacea. This connection remains controversial and not fully proven.
5. Environmental Triggers
- Sun Exposure: Ultraviolet (UV) radiation from the sun can trigger or worsen rosacea symptoms, leading to increased redness and inflammation.
- Temperature Extremes: Extreme heat or cold, as well as sudden temperature changes, can provoke flare-ups.
- Spicy Foods and Alcohol: Consuming spicy foods, hot beverages, and alcohol can trigger flushing and exacerbate symptoms.
6. Hormonal Factors
- Hormonal Changes: Hormonal fluctuations, such as those related to menopause or stress, might influence the severity of rosacea. The condition is more common in women, particularly in middle age.
7. Skin Care and Cosmetic Products
- Irritating Products: Harsh skincare products, including those with alcohol or other irritating ingredients, can exacerbate rosacea symptoms.
8. Lifestyle Factors
- Stress: Emotional or psychological stress may trigger or worsen rosacea symptoms. Managing stress can be an important part of controlling the condition.
9. Other Contributing Factors
- Genetic Predisposition: Certain genetic factors might make some individuals more susceptible to developing rosacea.
- Gut Health: Some research suggests that gut health and gastrointestinal issues may have an indirect effect on rosacea, although this connection is still being explored.
While these factors can contribute to the development of rosacea, they do not necessarily cause the condition in every individual. The interplay of these factors likely varies from person to person. If you suspect you have rosacea or are experiencing symptoms, consulting a dermatologist is essential for accurate diagnosis and management.
Types
Rosacea is a complex condition with several subtypes, each characterized by distinct symptoms and features. Here’s an overview of the different types of rosacea:
1. Erythematotelangiectatic Rosacea (Subtype 1)
- Primary Features:
- Facial Redness: Persistent redness in the central part of the face, often appearing as a flush or sunburn.
- Visible Blood Vessels: Small, dilated blood vessels (telangiectasia) on the cheeks, nose, and chin.
- Skin Sensitivity: The skin may feel sensitive or sting, especially in response to temperature changes, skincare products, or sun exposure.
- Symptoms: The redness and visible blood vessels may be accompanied by a sensation of heat or burning in the affected areas.
2. Papulopustular Rosacea (Subtype 2)
- Primary Features:
- Acne-like Breakouts: Red, swollen bumps that resemble acne, sometimes with pus-filled pustules.
- Persistent Redness: A red base often visible between and around the bumps.
- Swelling: Some individuals may experience facial swelling, particularly around the cheeks and eyes.
- Symptoms: The condition may cause skin texture changes with inflammation and swelling.
3. Phymatous Rosacea (Subtype 3)
- Primary Features:
- Thickened Skin: Significant thickening of the skin, often on the nose (rhinophyma), leading to a bulbous appearance.
- Texture Changes: The skin may become rough, bumpy, and irregular.
- Nasal Congestion: In severe cases, the thickening can affect nasal airflow.
- Symptoms: This subtype is more common in men and can lead to noticeable changes in facial features due to skin growth.
4. Ocular Rosacea (Subtype 4)
- Primary Features:
- Eye Irritation: Burning, stinging, or itching sensations in the eyes.
- Red or Bloodshot Eyes: The eyes may appear red or bloodshot.
- Dryness: A gritty or dry feeling in the eyes, leading to frequent blinking.
- Eyelid Issues: Inflammation of the eyelids (blepharitis) or conjunctivitis (pink eye) can occur.
- Symptoms: This subtype may lead to more serious complications if left untreated, including potential vision problems.
Other Considerations
- Flushing and Sensitivity: All subtypes of rosacea can involve episodes of flushing and increased skin sensitivity, which are common features across the condition.
- Combination of Subtypes: Some individuals may exhibit symptoms of more than one subtype simultaneously, making diagnosis and treatment more complex.
Management and Treatment
Each subtype of rosacea requires a tailored approach to management and treatment:
- Erythematotelangiectatic Rosacea: Treatment may include laser therapy to reduce visible blood vessels and topical medications to manage redness and sensitivity.
- Papulopustular Rosacea: Antibiotics (topical or oral) and medications that reduce inflammation can help manage acne-like breakouts.
- Phymatous Rosacea: Treatments may include surgical or laser procedures to reduce skin thickening and improve appearance.
- Ocular Rosacea: Eyelid hygiene, lubricating eye drops, and sometimes oral antibiotics can help manage eye symptoms.
Understanding the specific type of rosacea you have is crucial for effective treatment. Consulting a dermatologist is the best way to receive a proper diagnosis and personalized treatment plan.
Diagnosis
Diagnosing rosacea involves a comprehensive evaluation by a healthcare provider, typically a dermatologist. Here’s a detailed overview of the diagnostic process:
1. Medical History
- Symptom History: The dermatologist will ask about your symptoms, including when they started, how they have changed over time, and any triggers or factors that worsen the condition.
- Family History: Information about any family members with rosacea or similar conditions can be relevant.
- Medical History: The doctor will review your general health, any other skin conditions you may have, and any medications or treatments you are currently using.
2. Physical Examination
- Skin Examination: The dermatologist will closely examine your skin, particularly the face, to identify the characteristic features of rosacea, such as redness, visible blood vessels, bumps, and pustules.
- Assessment of Subtypes: The examination helps determine the subtype of rosacea (erythematotelangiectatic, papulopustular, phymatous, or ocular) based on the symptoms and skin changes observed.
3. Diagnostic Criteria
- Clinical Criteria: Diagnosis is primarily based on clinical criteria and visual inspection. The presence of certain key features (such as persistent facial redness, visible blood vessels, and acne-like breakouts) helps confirm the diagnosis.
- Symptom Pattern: The dermatologist will consider the pattern of symptoms, including their location, duration, and any episodic nature.
4. Differential Diagnosis
- Ruling Out Other Conditions: The dermatologist will differentiate rosacea from other skin conditions with similar symptoms, such as:
- Acne Vulgaris: Although rosacea can resemble acne, it typically lacks the blackheads and deep cysts found in traditional acne.
- Seborrheic Dermatitis: This condition can cause redness and scaling, but often affects different areas and has a different pattern.
- Lupus: Systemic lupus erythematosus can cause facial redness, but usually with additional systemic symptoms.
- Eczema: Atopic dermatitis (eczema) can cause redness and irritation but usually has a different appearance and pattern.
5. Additional Tests (if needed)
- Skin Biopsy: In rare cases, a skin biopsy might be performed to rule out other conditions or confirm the diagnosis, especially if the presentation is atypical.
- Eye Examination: For ocular rosacea, a thorough eye examination by an ophthalmologist may be necessary to assess the extent of eye involvement and manage symptoms effectively.
6. Diagnosis Confirmation
- Comprehensive Review: After reviewing the medical history, physical examination, and any additional tests, the dermatologist will confirm the diagnosis of rosacea and determine the subtype.
7. Treatment Plan
- Individualized Approach: Based on the subtype and severity of rosacea, the dermatologist will recommend a personalized treatment plan that may include topical or oral medications, lifestyle modifications, and skin care recommendations.
Early diagnosis and management are key to controlling rosacea and preventing long-term complications. If you suspect you have rosacea or are experiencing symptoms, consulting a dermatologist is the best course of action.
Treatment
Treating rosacea involves a combination of medical treatments, lifestyle changes, and skincare adjustments tailored to the specific subtype and severity of the condition. Here’s a comprehensive guide to the treatment options for rosacea:
1. Medical Treatments
Topical Medications
- Metronidazole: An anti-inflammatory and antimicrobial cream or gel that helps reduce redness and bumps.
- Azelaic Acid: Reduces inflammation, kills bacteria, and helps with acne-like breakouts.
- Ivermectin: An antiparasitic cream that helps reduce inflammation and acne-like lesions, particularly in cases with a high presence of Demodex mites.
- Brimonidine: A topical gel that constricts blood vessels to reduce redness.
Oral Medications
- Antibiotics:
- Doxycycline: An oral antibiotic with anti-inflammatory properties used to treat moderate to severe rosacea.
- Minocycline: Another oral antibiotic effective in managing rosacea symptoms.
- Isotretinoin: In severe cases, particularly those with nodular rosacea or persistent acne-like symptoms, isotretinoin (a powerful retinoid) may be prescribed. It’s usually reserved for cases that do not respond to other treatments due to its potential side effects.
Laser and Light Therapies
- Laser Therapy: Lasers, such as pulsed dye lasers, can help reduce visible blood vessels and redness.
- Intense Pulsed Light (IPL): IPL treatments target blood vessels and redness and can improve skin appearance by reducing inflammation and discoloration.
2. Skincare and Lifestyle Adjustments
Skincare Routine
- Gentle Cleansing: Use a mild, non-irritating cleanser to avoid exacerbating redness and sensitivity.
- Moisturizing: Apply a fragrance-free moisturizer to help maintain skin hydration and reduce dryness and irritation.
- Sun Protection: Daily use of broad-spectrum sunscreen with SPF 30 or higher is essential to protect the skin from UV radiation, which can trigger rosacea flare-ups.
Avoiding Triggers
- Identify Triggers: Keep a diary to track potential triggers such as spicy foods, hot beverages, alcohol, extreme temperatures, and stress.
- Avoid Known Triggers: Make lifestyle changes to avoid or minimize exposure to known triggers.
Diet and Lifestyle Changes
- Healthy Diet: Eating a balanced diet with plenty of fruits, vegetables, and whole grains can help manage rosacea. Avoiding trigger foods can prevent flare-ups.
- Stress Management: Techniques such as mindfulness, meditation, or yoga can help manage stress, which can exacerbate rosacea.
3. Management of Ocular Rosacea
- Eyelid Hygiene: Regular cleaning of the eyelids with gentle, non-irritating wipes or solutions to manage blepharitis and inflammation.
- Lubricating Eye Drops: Over-the-counter or prescription eye drops can help relieve dryness and irritation.
- Antibiotics: Oral or topical antibiotics may be prescribed for severe ocular rosacea to manage inflammation and infection.
4. Long-term Management
- Regular Follow-ups: Regular check-ins with a dermatologist to monitor progress and adjust treatment as needed.
- Consistency: Adhering to prescribed treatments and maintaining lifestyle modifications are key to managing symptoms effectively.
5. Supportive Measures
- Educational Resources: Learning about rosacea and connecting with support groups or organizations can provide additional resources and support.
Conclusion
Treating rosacea effectively requires a multi-faceted approach tailored to the individual’s specific symptoms and subtype. Collaboration with a dermatologist to develop a personalized treatment plan is crucial for managing the condition and improving quality of life.
Management and Prevention
Managing rosacea involves a combination of medical treatment and lifestyle adjustments:
- Sun Protection: Daily use of broad-spectrum sunscreen with at least SPF 30 can prevent sun-induced flare-ups.
- Avoiding Triggers: Identifying and avoiding personal triggers is crucial. Keeping a diary of flare-ups can help pinpoint specific causes.
- Gentle Skin Care: Using mild skin care products and avoiding harsh treatments can prevent irritation.
Prognosis
Rosacea is a chronic condition, and while it can be managed effectively, it often requires ongoing treatment and lifestyle adjustments. The severity of symptoms can vary, and with proper management, many people can achieve significant improvement in their condition.
If you have specific concerns about rosacea or its treatment, it’s best to consult a dermatologist who can provide personalized advice and treatment options.
